Change in IPR-V3 score

References
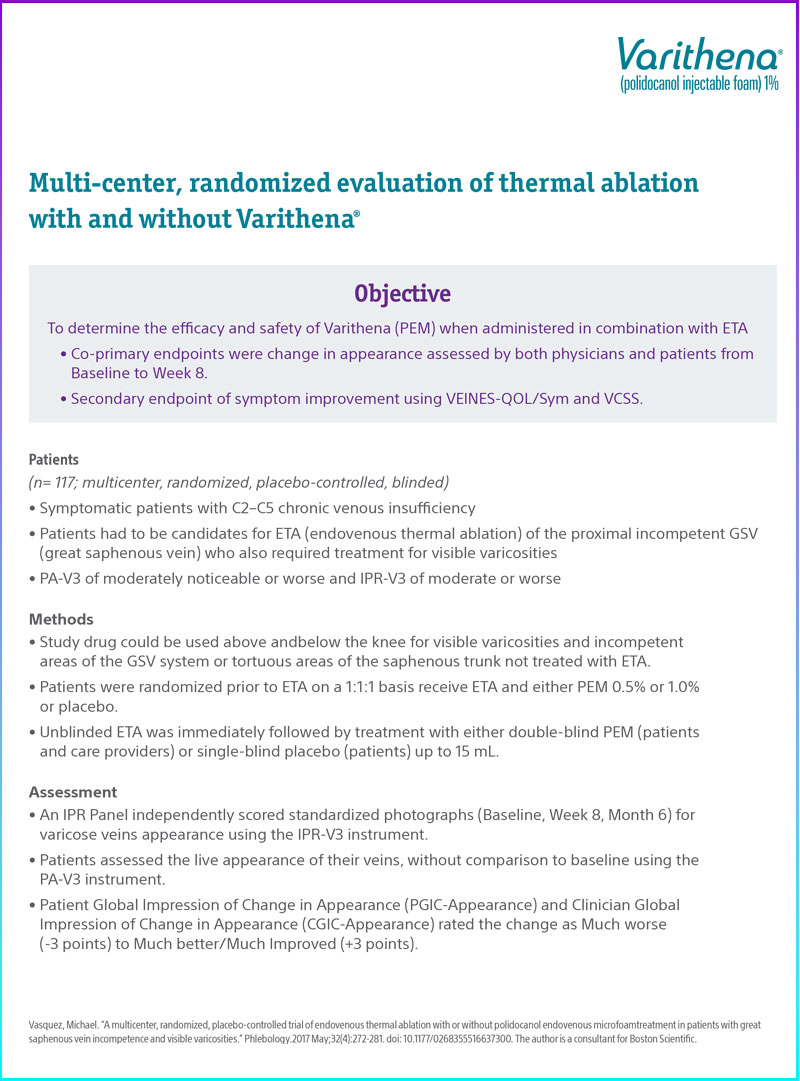
Vasquez, Michael. “A multicenter, randomized, placebo-controlled trial of endovenous thermal ablation with or without polidocanol endovenous microfoam treatment in patients with great saphenous vein incompetence and visible varicosities.” Phlebology.2017 May;32(4):272-281. doi: 10.1177/0268355516637300. The author is a consultant for Boston Scientific.