References
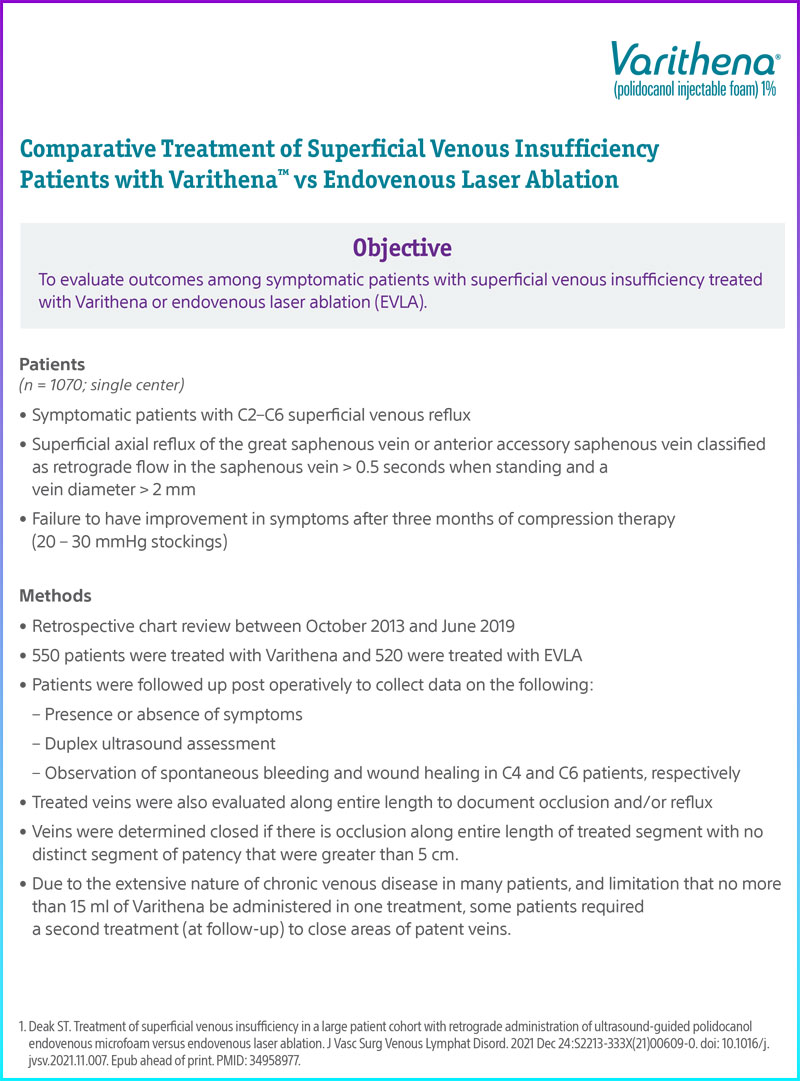
Deak ST. Treatment of superficial venous insufficiency in a large patient cohort with retrograde administration of ultrasound-guided polidocanolendovenous microfoam versus endovenous laser ablation. J Vasc Surg Venous Lymphat Disord. 2021 Dec 24:S2213-333X(21)00609-0. doi: 10.1016/j.jvsv.2021.11.007. Epub ahead of print. PMID: 34958977.