References
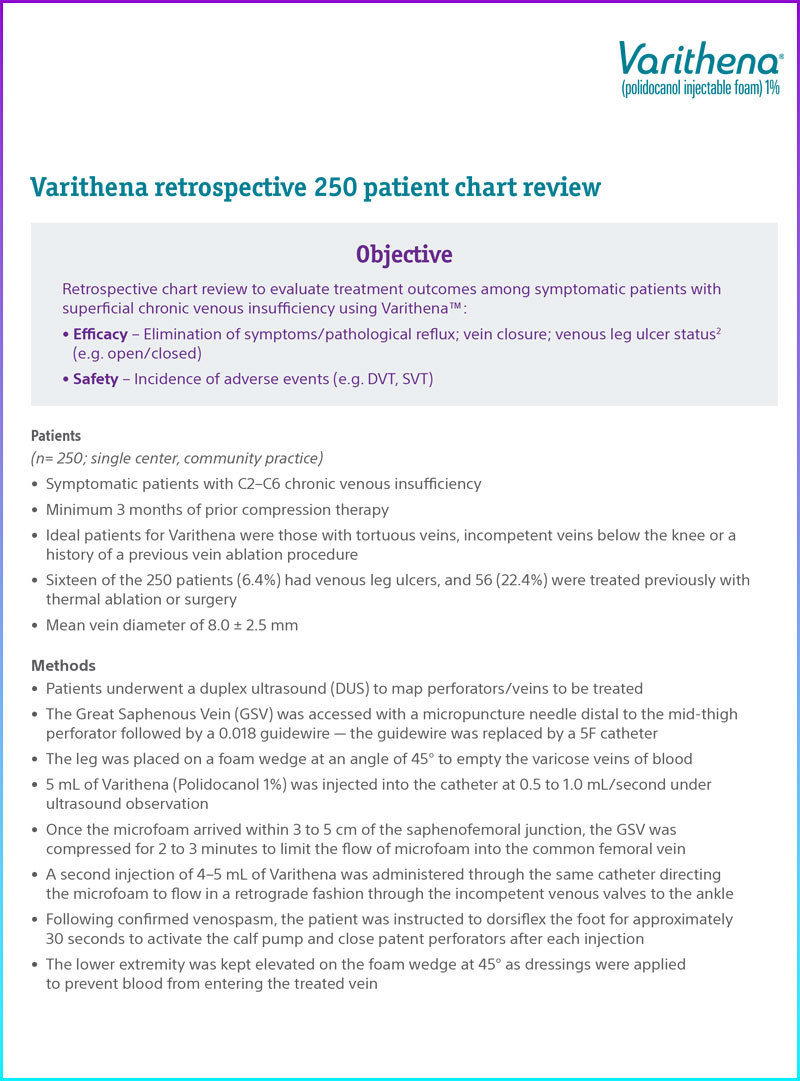
Deak, Steven T. “Retrograde Administration of Ultrasound-Guided Endovenous Microfoam Chemical Ablation for the Treatment of Superficial Venous Insufficiency.” Journal of Vascular Surgery: Venous and Lymphatic Disorders, vol. 6, no. 4, July 2018, pp. 477–484., doi:https://doi.org/10.1016/j.jvsv.2018.03.015. The author is a consultant for Boston Scientific.
1. Healing of venous leg ulcers was not an endpoint in Varithena pivotal trials.